The Comprehensive Guide to Navigating Cancer: Information, Support, and Resources for Patients and Families
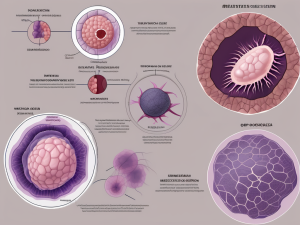
Cancer can change your life in many ways, but understanding your diagnosis, knowing your treatment options, and connecting with support can empower you to face these challenges with hope and strength. Whether you are a patient, caregiver, or family member, this guide offers reliable information and practical advice to help you navigate the complex cancer […]