The Power of Low-Dose CT Scans in Early Lung Cancer Detection
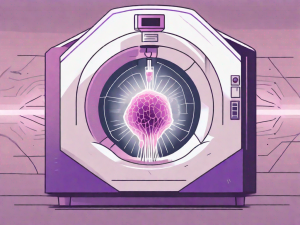
Early detection of lung cancer can save lives, and low-dose CT (LDCT) scans are transforming how we find lung cancer early—when treatment is most effective. If you or a loved one has a history of heavy smoking or are between 50 and 80 years old, LDCT screening could be a crucial step in protecting your […]