Melanoma is a serious form of skin cancer influenced by both sun exposure and genetic factors. While harmful ultraviolet (UV) rays are a well-known cause, gene mutations can also increase your risk—even if you limit your time in the sun. Understanding how genetics affects melanoma risk can help you take proactive steps, whether through careful skin monitoring, genetic testing, or preventive care. This article walks you through the basics of melanoma, key genetic markers like CDKN2A and BRAF, strategies for early detection, and ways to protect your skin for a healthier future.
What Is Melanoma and Why Should You Care?
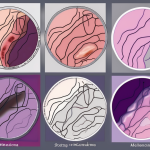
Melanoma starts in melanocytes, the skin cells that give your skin its color. Sometimes, these cells grow uncontrollably, forming cancer. It can develop anywhere on your skin—even places not usually exposed to sunlight. Early detection is crucial because melanoma can spread to other parts of your body if left unchecked. You can protect yourself by regularly checking your skin for any new or changing moles or spots.
Look for signs using the ABCDE rule:
- Asymmetry: One half of a mole doesn’t match the other
- Border: Edges are irregular, ragged, or blurred
- Color: Varies in shades or has multiple colors
- Diameter: Larger than a pencil eraser (about 6 mm)
- Evolving: Changes in size, shape, or color over time
If you notice any of these changes, consult a dermatologist promptly.
Risk Factors: How Sun and Genes Increase Your Chances
Everyone’s risk of melanoma is different, often based on a combination of lifestyle and inherited factors. Too much UV radiation from the sun or tanning beds can damage your skin cells and increase melanoma risk. But genetics also play a big role. If you have fair skin, many moles (especially unusual ones), or a family history of melanoma, your risk is higher.
Key Genetic Factors in Melanoma
Scientists have identified several gene mutations linked to melanoma, which can help explain why some people get melanoma despite limited sun exposure.
- CDKN2A: This gene helps control cell growth. Mutations here can remove the brakes on melanocyte growth, increasing melanoma risk. If melanoma runs in your family, genetic testing for CDKN2A mutations might be advised.
- BRAF: Found in many melanoma tumors, mutations in BRAF affect how cells grow and divide. Targeted therapies now exist for melanomas with BRAF mutations.
- MC1R: This gene influences skin and hair color. Certain variants are linked to red hair, fair skin, and increased melanoma susceptibility.
- TP53: Known as the “guardian of the genome,” this gene helps fix DNA damage. Mutations can lead to cancer development.
Knowing your genetic makeup can guide personalized screening and prevention plans.
How Genetic Testing and Counseling Can Help You
If melanoma runs in your family or you have many atypical moles, consider seeing a genetic counselor. They can explain your risk, advise on testing, and help you interpret results. For those with confirmed gene mutations like CDKN2A, regular skin exams, mole mapping, and avoiding UV exposure become even more critical.
Protecting Your Skin: Prevention Tips That Work
While you can’t change your genes, you can control how much sun damage your skin takes. Here’s how:
- Use broad-spectrum sunscreen with SPF 30 or higher daily, even on cloudy days (Mayo Clinic Sun Protection Guide)
- Wear protective clothing, wide-brimmed hats, and UV-blocking sunglasses
- Seek shade, especially between 10 a.m. and 4 p.m. when UV rays are strongest
- Avoid tanning beds completely
- Check your skin monthly; use mirrors or ask someone to help examine hard-to-see areas
Regular Dermatologist Visits Matter
Alongside self-checks, see a dermatologist annually or as recommended based on your risk. These experts can detect early melanoma signs you might miss and perform biopsies when needed.
Taking Charge of Your Skin Health
Understanding melanoma’s genetic and environmental factors empowers you to act early and reduce risks. If you have a family history of melanoma or notice skin changes, don’t delay in seeking professional advice. Early detection saves lives by allowing treatment before melanoma spreads.
For more detailed information, visit the National Cancer Institute’s melanoma page or watch educational videos from Cancer Research UK.
Frequently Asked Questions
1. How do I know if my moles are suspicious?
Use the ABCDE rule to check for asymmetry, irregular borders, multiple colors, size larger than 6 mm, or changes over time. Any mole showing these signs should be evaluated by a dermatologist.
2. Who should consider genetic testing for melanoma risk?
If you have a strong family history of melanoma, multiple atypical moles, or a personal history of melanoma at a young age, genetic testing—especially for CDKN2A mutations—could be helpful.
3. Can melanoma develop in areas not exposed to the sun?
Yes. While sun exposure increases risk, melanoma can also appear in less-exposed areas, like under fingernails or on the soles of your feet.
4. Is melanoma always fatal?
No. When found early, melanoma is highly treatable and often curable with surgery. Advanced melanoma treatment has also improved thanks to targeted therapies.
5. How often should I have my skin checked by a professional?
Most people benefit from an annual skin exam, but if you have increased risk factors, your doctor may recommend more frequent visits.