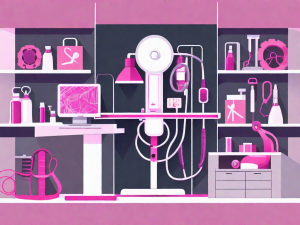
A Guide to Breast Self-Exams for Cancer Screening
Breast self-exams are the easiest tool for keeping a track of your breast-health. By regularly examining your breasts, you become familiar with their normal look and feel, making it easier to spot any changes that may occur. It’s a simple and effective method that every woman should incorporate into her routine. In this comprehensive guide, we will walk you through everything you need to