Advancements in Cancer Blood Test: A Game-Changer in Early Detection
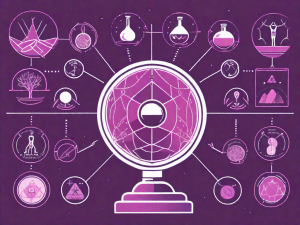
This article highlights the transformative role of advanced cancer blood tests in early diagnosis and management. Emphasizing the critical importance of early detection, it explains how these non-invasive blood tests, also known as liquid biopsies, are revolutionizing cancer care. By detecting biomarkers like circulating tumor cells or DNA in the blood, these tests offer a less